You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Although aging is not a cause of tooth loss, the incidence increases with age. Currently, the elderly make up the largest growing segment of American society. In most industrialized countries, the rate of edentulism is decreasing at a rate of 1% per year. However, the shear increase in overall population numbers in this segment of society has resulted in a general rise in the number of edentulous individuals. In the United States alone, it is predicted that, although people are now keeping their teeth longer than in the past, there will be approximately 38 million edentulous elderly adults by the year 2020 compared with only 33.6 million in 1991; the aging of the “baby boom” population largely accounts for the increase.2 Consequently, the ongoing need to provide this segment of the population with treatment options for tooth replacement therapy is paramount. Although it has been argued that implant dentistry is the standard of care for this patient group,3 socioeconomic factors may prohibit some segments of the population from the desire and/or ability to seek such treatment modalities. Considering that the overall number of completely edentulous individuals is expected to increase over the years, removable prosthodontics will continue to be a necessary treatment modality in clinical dentistry.
Denture Fabrication
In the history of tooth replacement therapy, sophistication in treatment modalities was not afforded until recently. Since the early 19th century, the construction of complete dentures has involved a lost-wax/investment technique with teeth set in a wax-trial denture, then encompassed by an investment material, with the wax ultimately replaced by a definitive denture base material. From the mid-1850s, the material of choice was Vulcanite. In the 1930s, this was superseded by acrylic resin: polymethylmethacrylate (PMMA).4 PMMA continues to be the material of choice for the fabrication of complete dentures. Although significant advances have been made in material formulations and laboratory technique, the overall physical and mechanical properties of modern PMMA formulations fail to fulfill all the ideal requirements as described by Anusavice.5
The laboratory process of denture fabrication has not deviated significantly since the 1930s. As it does now, the process then involved the use of paired flasks to create molds of the wax-trial denture set-up, followed by removal of the wax (boil-out), placement of mixed PMMA dough, flask trial closure, processing in a hot water bath, and finally divesting/break-out, trim, and polish. The most significant advances have been in the delivery of the mixed PMMA dough. Dentures processed via injection-molded systems now have the capability of producing greater accuracy and dimensional stability than those produced via standard compression techniques.6,7 The injection technique also affords smoother surface characteristics.8
The most notable paradigm shift in denture base acrylic and associated fabrication/processing techniques occurred in 2002 with the introduction of a light-curable, thermoplastic urethane-dimethacrylate prosthetic resin system. This system replaces the lost wax-technique. Some of its advantages include not using monomer (methyl, ethyl, butyl, or propyl methacrylate); elimination of flasking and packing; short processing times; and less than half of the volumetric curing shrinkage when compared to conventional PMMA.9 Another benefit is that regular PMMA denture base materials can bond to urethane dimethacrylate. Consequently, a separate denture base in either clear or tissue-colored material can be fabricated, which can then be used with conventional wax-trial denture set-ups and PMMA materials to become an integral part of the final prosthesis.9,10 Limitations include the requirement for a heating/conditioning oven, the proprietary/specific light oven; the electric heating instrumentation; and the mechanical retention slots/diatorics in acrylic teeth (due to lack of chemical bonding) and/or use of a special bonding agent. Also, as with most new technologies, there is a learning curve for both the dental technician and dentist using these materials.
Clinical Techniques
Clinical techniques involved in denture fabrication have not changed significantly over the years. Although specific techniques may vary from operator to operator, the overall goals remain the same: denture support, retention, and stability. In order to achieve satisfactory support from the overlaying prostheses, accurate impression techniques that capture the underlying bone and soft tissues are required. Retention is a function of capturing passive peripheral extensions affording a peripheral seal. Stability is a consequence of a satisfactory occlusal scheme and maxillo-mandibular relations.
There are three basic concepts for impression-making, based on pressure applied to various anatomical areas: mucostatic impression technique (minimal pressure technique); functional impression technique (pressure technique); and semi-functional impression technique (selective-pressure technique). Of these techniques, the most popular method taught in the undergraduate dental setting is the selective-pressure technique. This approach attempts to place most stress on those areas of the maxilla and mandible that can best resist functional forces of the denture bases. Other popular techniques include the use of a custom tray, border molding with modeling plastic impression compound or elastomeric impression material (polyvinyl siloxane or polyether), vent holes, selective wax-relief, and the “open-mouth” impression approach.11
Conventional clinical appointment sequence in complete denture fabrication is as follows:
Appointment 1: Examination, diagnosis, initial impressions.
Appointment 2: Secondary impressions.
Appointment 3: Maxillo-mandibular jaw relation records (both centric and vertical relation). Tooth selection.
Appointment 4: Wax-trial denture try-in.
Appointment 5: Delivery of definitive prostheses.
The impression techniques described above all subscribe to the use of custom impression trays. These are constructed on primary casts generated from initial impressions taken during the first clinical appointment. The resources used include either auto- or light-polymerized resin tray materials. However, manufacturers have introduced products to combine some of these clinical steps in denture fabrication with stock, modifiable tray/wax rim products. For example, a thermoplastic prefabricated tray material with a prepositioned occlusion wax rim attached mechanically to the tray is available. The tray material can be manipulated, molded, and trimmed once heated and customized intraorally or on a cast generated from an initial impression. Once adjusted, a secondary impression is taken using border-molding techniques and materials familiar to the operator. The wax rims are then adjusted to the correct vertical and horizontal dimensions, and jaw relation/facebow transfer records are taken. Although these products and associated techniques have the potential to reduce overall clinical time by combining the first three visits in the conventional sequence of clinical appointments,12 there is no literature to support or disprove the efficacy of treatment outcomes with this approach.
Denture Teeth
Along with advances in denture base materials and processing techniques, manufacturers continue to develop and introduce tooth lines with improved esthetics and mechanical properties.13 Some teeth lines are manufactured with a layering process that uses a triple-cross-linked PMMA resin and microfilled materials for improved wear resistance. Other manufacturers have introduced nano-hybrid composite technology into the tooth manufacturing process. These teeth will bond to PMMA base materials without any special bonding agent. Examples include the Phonares® tooth line (Ivoclar Vivadent Inc, www.ivoclarvivadent.us) and the Mondial® tooth line (Kulzer, www.kulzer.com).
Denture Esthetics and Anterior Tooth Selection and Arrangement
Denture esthetics has essentially involved a subjective approach, employing long-standing techniques and principles to help reach a satisfactory esthetic and functional outcome for the patient and dental team. Particularly, this is the case with the clinical arrangement of the teeth in the trial-denture base. Although there have been no significant advances in recent years, such principles have been well-described elsewhere.14
Posterior Anatomy and Occlusion
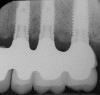
Posterior tooth selection and arrangement varies depending on prescribed theories and operator preference. The two most popular posterior occlusal scheme relationships are conventional buccalized occlusion and lingualized occlusion. Posterior lingualized occlusion is not a recent concept.15,16 It involves paring a maxillary high-degree cuspal plane posterior tooth shape (eg, 33º) with an opposing lower-degree (eg, 0º to 22º) cuspal plane posterior tooth line (Figure 1 through Figure 4). The maxillary palatal cusp alone is placed in contact with the opposing teeth, providing support and function. It is essentially a “mortar and pestle” action. Purported benefits of lingualized posterior occlusal schemes include improved food bolus penetration and the potential to reduce the vertical forces placed on the residual alveolar ridges.15,16 However, there is little evidence in the literature to support such claims. In a recent randomized, controlled study performed by Sutton and McCord,17 patients were allocated different dentures with the following posterior tooth arrangement: 0º; anatomic posterior teeth (33º cuspal angle) and lingualized occlusion teeth. Patients reported no significant differences in chewing capability and overall comfort and satisfaction between lingualized occlusion teeth and anatomic teeth. However, when wearing 0º teeth, patients reported higher overall oral discomfort and difficulty in eating.
Regardless of the lack of clinical studies to support lingualized over buccalized occlusal schemes, lingualized occlusal concepts have been gaining recent popularity as evidenced by manufacturers devoting new posterior tooth mold lines specifically to this occlusal scheme.
CAD/CAM
CAD/CAM techniques have provided significant benefits and improvements in fixed prosthodontics. However, up until recently, this has not been the case in the removable field. The most notable exception is the use of CAD/CAM design and manufacturing principles in the fabrication of posterior teeth. With this approach, teeth are produced with high levels of accuracy and uniformity, making it possible to produce precisely matched pairs of teeth. This has allowed Heraeus to develop and release a novel method of posterior tooth set-up that uses these CAD/CAM-generated teeth with a jig system and specially designed articulator—the Filou 28™ Denture set-up system (Figure 5 through Figure 8). The jig system allows for anatomically correct positioning of the posterior teeth relative to each other, using specially customized posterior tooth impression blocks. Advantages include standardization of posterior tooth set-ups, accurate occlusal arrangement, and time-savings in the set-up process.
Dental Implant Therapy
A discussion of updates in removable complete denture therapy would not be complete without referencing dental implant therapy. In fact, it is the author’s opinion that complete denture therapy is the gateway to implant therapy—an ever-growing treatment modality in clinical dentistry.
Significant advances in implant dentistry continue to provide benefits for the partially edentulous population. However, it is in the completely edentulous patient group that significant benefits are realized. These include but are not limited to:
- preservation of bone and subsequent muscle attachment.18,19
- increased prostheses support, retention, and comfort.20
- increased masticatory ability.21,22
- increased confidence: psychological benefit.23
In essence, these benefits have the potential to improve quality of life for the prospective patient.
In overdenture therapy, prosthetic design can be divided into two groups: stress-broken and rigid. Stress-broken prostheses require fewer implants, with attention to biomechanical design features to allow for rotation (stress-breaking) of the prostheses around the implant locations. These prostheses are essentially tissue-supported and implant-retained. They replace the adhesive/glue, providing needed retention, comfort, and support. An example would include two implants in site Nos. 23 and 26, with either solitary anchor systems (ball or stud attachments) or a splinted bar-overdenture design (Figure 9 through Figure 11). Masticatory function is improved and patient satisfaction increased. Rigid prostheses require multiple implants, with the forces being transferred from the supra-infrastructure directly to the implants. These prostheses are implant-supported and implant-retained. The design can be removable or fixed (Figure 12 through Figure 16), depending on patient- and operator-mediated preferences.24-27 Within the fixed group of prostheses, materials used may vary from acrylic-fused-to-metal, porcelain-fused-to-metal, or all-ceramic. The cost of these material choices varies significantly, with acrylic options providing the most affordable, entry-level approach for the patient.14
Conclusion
As the baby boomer population in the United States ages, the overall incidence of complete edentulism will also rise. This segment of the population will be seeking treatment options that may or may not involve implant therapy. In either situation, a skill set in complete denture fabrication is paramount. Along with advances in the material characteristics, processing techniques, and posterior tooth
arrangement possibilities, the field of removable prosthodontics will continue to have a significant and rewarding role in modern dentistry.
References
1. Mojon P. The world without teeth: demographic trends. In: Feine JS, Carlsson GE, eds. Implant Overdentures: the standard of care for edentulous patients. Hanover Park, Ill: Quintessence Publishing; 2003:3-14.
2. Douglass CW, Shih A, Ostry L . Will there be a need for complete dentures in the United States in 2020? J Prosthet Dent. 2002;87(1):5-8.
3. Feine JS, Carlsson GE, Awad MA, et al. McGill consensus conference statement on overdentures. Montreal, Quebec, Canada. May 24-25, 2002 . Int J Prosthodont. 2002;15(4):413-414.
4. Stafford GD, Smith DC. Some studies of the properties of denture base polymers . Br Dent J. 1968;125(8):337-342.
5. Anusavice KJ . Phillips’ Science of Dental Materials. 11th ed. St. Louis, MO: W.B. Saunders; 2003.
6. Nogueira SS, Ogle RE, Davis EL. Comparison of accuracy between compression- and injection-molded complete dentures . J Prosthet Dent. 1999;82(3):291-300.
7. Craig RG, Powers JM, eds . Restorative Dental Materials. 11th ed. St. Louis, MO: Mosby; 2001.
8. McCord JF. Contemporary techniques for denture fabrication . J Prosthodont. 2009;18(2):106-111.
9. Kurtzman GM, Melton AB. Full arch removable prosthetics with Eclipse . Spect Denturism. 2008;2(1):1-8.
10. Wagner SA. Increasing patient satisfaction and practice efficiencies via clear-base removable dentures . Pract Proced Aesthet Dent. 2008;20(2 Suppl):S2-S7.
11. Petropoulos VC, Rashedi B. Current concepts and techniques in complete denture final impression procedures . J Prosthodont. 2003;12(4):280-287.
12. Krantz WA, Adrian ED, Ivanhoe JR. Combining final impressions and the centric jaw relation records into one appointment using an irreversible hydrocolloid blockout technique . J Prosthet Dent. 1991;66(6):821-822.
13. Ghazal M, Steiner M, Kern M. Wear resistance of artificial teeth . Int J Prosthodont. 2008;21(2):166-168.
14. Leopardi A. Complete dentures: achieving superior anterior esthetics and post-delivery maintenance . Inside Dentistry. 2009;6(7):70-80.
15. Parr GR, Loft GH. The occlusal spectrum and complete dentures . Compend Contin Educ Dent. 1982;3(4):241-250.
16. Becker CM, Swoope CC, Guckes AD. Lingualized occlusion for removable prosthodontics . J Prosthet Dent. 1977;38(6):601-608.
17. Sutton AF, McCord JF. A randomized clinical trial comparing anatomic, lingualized, and zero-degree posterior occlusal forms for complete dentures . J Prosthet Dent. 2007;97(5):292-298.
18. Wright PS, Glantz PO, Randow K, et al. The effects of fixed and removable implant-stabilised prostheses on posterior mandibular ridge resorption . Clin Oral Implants Res. 2002;13(2):169-174.
19. Burns DR. Mandibular implant overdenture treatment: consensus and controversy . J Prosthodont. 2000;9(1):37-46.
20. Sadowsky SJ. Treatment considerations for maxillary implant overdentures: a systematic review . J Prosthet Dent. 2007;97(6):340-348.
21. Garrett NR, Ancowitz S, Sze S, et al. Effects of implant/tissue support of dentures on masticatory performance . J Dent Res. 2008:625.
22. Fueki K, Kimoto K, Ogawa T, et al. Effect of implant-supported or retained dentures on masticatory performance: a systematic review . J Prosthet Dent. 2007;98(6):470-477.
23. Zitzmann NU, Marinello CP. Treatment outcomes of fixed or removable implant-supported prostheses in the edentulous maxilla. Part I: patients’ assessments . J Prosthet Dent. 2000;83(4):424-433.
24. Bidez MW, Misch CE. Force transfer in implant dentistry: basic concepts and principles . J Oral Implantol. 1992;18(3):264-274.
25. Ranger B, Krogh PH, Langer B, Van Roekel N. Bending overload and implant fracture: a retrospective clinical analysis . Int J Oral Maxillofac Implants. 1995;10(3):326-334.
26. Benzing UR, Gall H, Weber H. Bio-mechanical aspects of two different implant-prosthetic concepts for the edentulous maxillae . Int J Oral Maxillofac Implants. 1995;10(2):188-198.
27. Leopardi A. Fixed restorative options for the edentulous maxilla . Functional Esthetics & Restorative Dentistry. 2008;2(3):44-56.
About the Author
Aldo Leopardi, BDS, DDS, MS
Prosthodontist
Private Practice
Greenwood Village, Colorado